Mpox, caused by the monkeypox virus and related to the eradicated smallpox virus, typically manifests as skin rashes or lesions, accompanied by symptoms such as fever and muscle aches. Transmission occurs through direct contact with infected blood, body fluids, skin lesions or contaminated surfaces and objects.
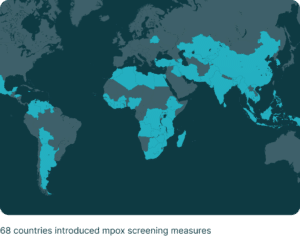
Mpox Clade I is endemic to Central Africa, while Clade II is found in West Africa, with the first human case reported in the DRC in 1970. The ongoing outbreak that began in May 2022 is predominantly driven by Clade II. Following a peak in 2022, cases declined by early 2023 but have persisted at low levels globally. From January 2022 to September 2024, the WHO recorded approximately 109,699 laboratory-confirmed cases across 123 countries. However, in 2024, the emergence of the Clade I strain intensified the outbreak, spreading mpox to previously unaffected areas of the DRC and neighbouring countries like Burundi, Rwanda and Uganda. Surveillance measures, including temperature checks and health declarations, were implemented at entry points in at least 68 countries, adding strain to already fragile healthcare systems.
The mpox virus is anticipated to remain a concern for global health in 2025, given the Clade I outbreak in Central and Eastern Africa. Effective mitigation will require rapid detection and improved vaccination efforts, though vaccine distribution and regulatory hurdles will challenge containment efforts.
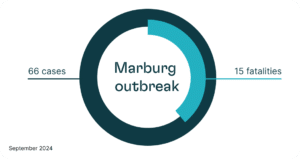
Marburg virus outbreak
The Marburg virus, a rare but deadly hemorrhagic fever virus related to Ebola, also poses a growing global health threat. A recent outbreak in Rwanda since September 2024, the third largest outbreak to date, with 66 confirmed cases and 15 fatalities, highlights the need for robust surveillance and rapid response. While there is no specific treatment for the disease and vaccine trials are still ongoing, early detection, containment, rehydration and symptom management can improve survival rates, especially for high-risk groups such as healthcare workers and those in close contact with infected individuals. The virus is typically transmitted from fruit bats to humans or through human-to-human contact, with climate change and deforestation heightening exposure risks. As research into vaccines and treatments continues, international cooperation is essential to prevent further outbreaks and protect vulnerable populations.